Losing a tooth can feel like more than just a cosmetic issue. Behind the scenes, the jawbone where the tooth once sat can begin to shrink and weaken. That’s where the question comes in—what is a bone graft for teeth?
A bone graft is a minimal surgical procedure that helps restore and regenerate bone in areas where it has deteriorated or thinned. It’s often a critical first step before getting dental implants or restoring your oral function. Bone grafting sounds intense, but in the right hands, it’s a manageable, low-risk step toward better oral health.
Who Might Need a Bone Graft?
Not everyone with missing teeth will need a bone graft. But there are a few scenarios where this procedure becomes essential. If your jawbone has started to lose density or volume, chances are, your dentist might recommend one.
Let’s walk through who typically benefits from this procedure:
- People with missing teeth for more than a few months or years
- When you lose a tooth, the bone no longer receives the stimulation it needs. Eventually, it starts to deteriorate.
- Patients preparing for dental implants
- Implants need a strong foundation. A graft creates the structure required to hold the implant securely.
- Trauma patients
- Facial injuries or accidents can lead to bone damage. Bone grafts help restore the jaw’s original form.
- Gum disease sufferers
- Advanced periodontitis doesn’t just affect your gums—it eats away at the bone beneath. A graft helps repair the loss.
- Sinus lift candidates
- For implants in the upper jaw, specifically the back molars, a sinus lift and graft may be necessary to build adequate bone height.
Even though the idea of bone grafting may sound intimidating, many patients undergo the procedure comfortably with local anesthesia or sedation. It’s not as dramatic as it seems, especially when performed by an experienced local dentist or a dentist in Petaluma, CA.
Key Signs You Might Be a Candidate for a Bone Graft
Wondering if this procedure is something you might need? While your dentist will ultimately decide, here are some common indicators:
1. Tooth Loss Without Replacement
Have you been missing a tooth for several months or even years?
Bone loss typically begins soon after a tooth is lost and continues over time. If you’re thinking about getting an implant now, your jawbone may not have enough volume left to support it.
2. Loose Dentures or Bridges
When dentures no longer fit snugly or feel like they’re “floating,” it could mean your jawbone has changed shape. As bone recedes, the contours of your jaw shift, leading to poor denture fit and discomfort.
Signs to watch for:
- Dentures slipping during speech or eating
- Pressure sores in your mouth
- Needing frequent adjustments
3. Gum Recession or Bone Exposure
Sometimes, gum loss reveals more serious bone issues. If your teeth appear longer than before, or you see exposed roots, there may be significant bone loss underneath.
This is especially common with chronic gum infections and advanced periodontal disease.
4. Jaw Pain or Facial Changes
Did your face begin to look “sunken in” over time?
Bone loss can affect the lower half of your face, making you appear older. Some people also experience mild jaw pain or notice a change in bite alignment due to shifting teeth.
These are signs that the supporting bone structure is weakening.
5. You’ve Been Told You’re Not a Good Candidate for Implants
Have you been excited about dental implants only to hear, “You don’t have enough bone”?
That doesn’t have to be the end of the road.
A bone graft builds the foundation needed for implant surgery. Many patients go on to receive successful implants after a graft.
6. History of Dental Trauma or Infection
If you’ve suffered trauma, had a cyst or abscess removed, or undergone tooth extraction due to infection, chances are the area may lack sufficient bone. Bone grafting restores what was lost and helps avoid further complications.
What Happens During a Bone Graft?
Curious about the procedure itself? Here’s a quick breakdown:
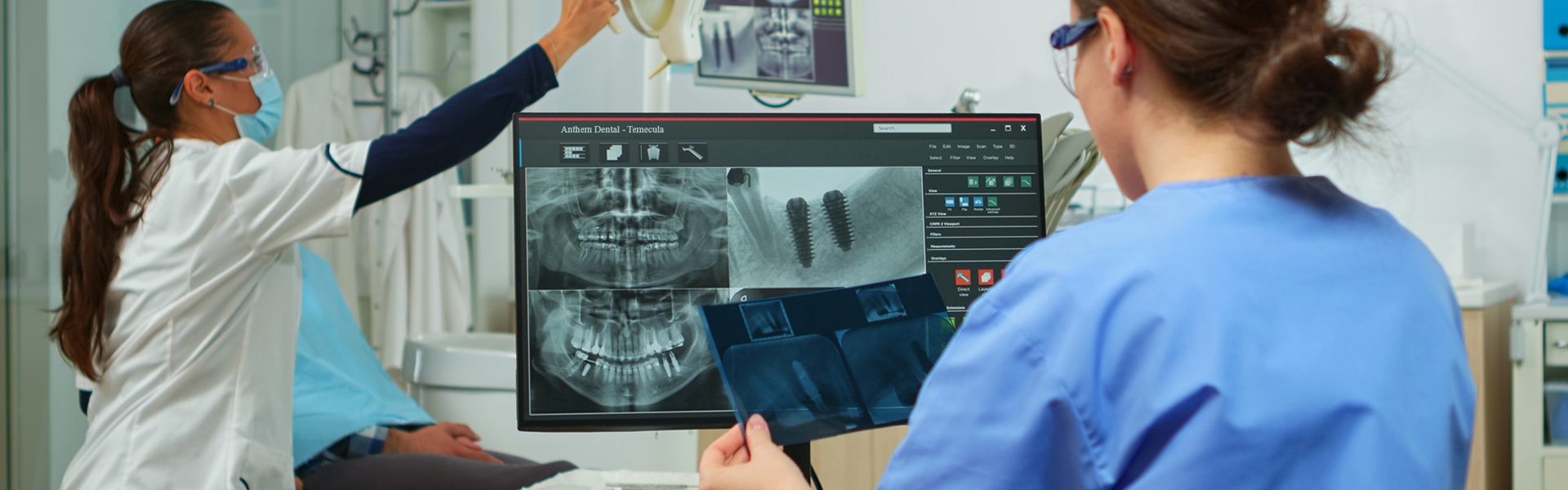
- Assessment – Your dentist takes X-rays or 3D scans to measure bone density.
- Preparation – The site is numbed, and the area is cleaned.
- Placement – Bone material (from your body or synthetic) is carefully inserted.
- Healing – Over several months, your body integrates the graft and builds new bone.
It’s a routine part of oral surgery in Petaluma, CA, and can be performed right in the dental office with minimal downtime. Most patients from the locality go back to normal activities within a day or two.
Recovery and Aftercare
Don’t worry—it’s not as painful as it sounds. Recovery usually involves:
- Mild swelling or tenderness for a few days
- Prescription or over-the-counter pain relief
- Soft foods for a week or so
- Follow-up checkups to monitor progress
Keep the area clean, follow your dentist’s instructions, and you’ll be on your way to a stronger smile.
How Long Until You Can Get Implants?
Bone grafts need time to heal and integrate with your existing bone. Depending on the size and location of the graft, healing might take anywhere from 3 to 6 months.
Once healed, you’ll return to your dentist to plan the next step, often dental implant placement.
Conclusion
If you’ve lost a tooth or been told you don’t qualify for implants, you might be wondering, “What is a bone graft for teeth really about?” It’s not a scary procedure—it’s a smart one. It restores strength where your jawbone has weakened, giving you back the stability needed for lasting dental solutions.
At Petaluma Dental Group, you’re here to help patients rebuild confidence and oral health in a safe, comfortable environment. If you’re ready to explore your options or want a second opinion, now is a great time to book a consultation.